Chronic pain syndrome is a complex and often debilitating condition in which an individual experiences pain that persists for more than three months, despite medical treatment or other interventions.
The causes of chronic pain syndrome are not fully understood, but there are several factors that may contribute to its development. These can include physical injury or trauma, underlying medical conditions, changes in the nervous system, emotional factors, genetics, and lifestyle factors, exposure to electromagnetic fields exposure, pollutions…
What factors can explain chronic pain?
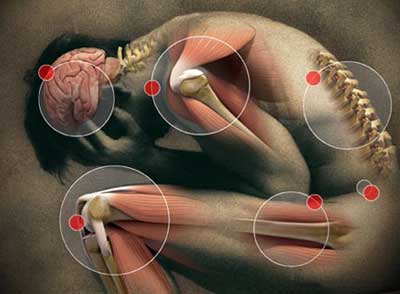
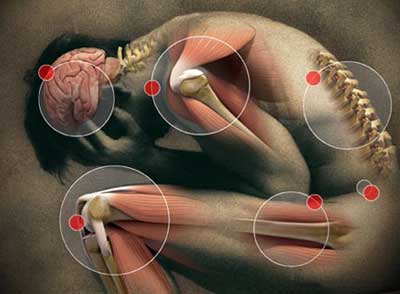
How nervous system can lead to chronic pain
The nervous system plays a critical role in the experience of chronic pain. Chronic pain can cause changes in the nervous system, leading to a state of hypersensitivity or hyperexcitability. These changes can occur at various levels of the nervous system, including the peripheral nerves, spinal cord, and brain. For example, in chronic pain conditions such as fibromyalgia, there is evidence of alterations in the processing of pain signals in the spinal cord and brain, leading to an increased sensitivity to pain.
Emotions…emotions
Emotional factors such as stress, anxiety, and depression can also contribute to the development and persistence of chronic pain. These emotional factors can cause changes in the brain’s limbic system, which is involved in the regulation of emotions and pain perception. Chronic stress, for example, can lead to an increase in the production of stress hormones such as cortisol, which can exacerbate inflammation and pain.


Genetics
Genetics may also play a role in the development of chronic pain syndrome. Some individuals may be genetically predisposed to conditions such as fibromyalgia or chronic migraines, which are associated with chronic pain. Certain genetic variations may also affect the way an individual processes pain signals or responds to treatment.
When you will decide to take care of you?
Lifestyle factors such as poor sleep, lack of exercise, and a diet high in processed foods and sugar can contribute to the development and persistence of chronic pain. Poor sleep, for example, can lead to changes in the levels of neurotransmitters such as serotonin and dopamine, which are involved in pain perception and mood regulation. Lack of exercise can lead to a decrease in muscle strength and flexibility, which can exacerbate pain.
Electromagnetic field…most are not aware of their effects
Finally, electromagnetic emissions have been studied as a potential factor in chronic pain. Some studies have suggested that exposure to electromagnetic fields (EMFs) may be associated with an increased risk of chronic pain. You can have some more information here
There are several studies about how electromagnetic emissions may be involved in chronic pain. One is that EMFs interfere with the body’s natural electrical and magnetic fields, which can disrupt the normal functioning of cells and tissues. This disruption may lead to inflammation and other changes that can contribute to chronic pain.


Another is that EMFs may affect the production and release of certain chemicals in the body, such as neurotransmitters and hormones, which can influence pain perception and sensitivity. For example, exposure to EMFs has been shown to increase the production of inflammatory cytokines, which can contribute to pain and inflammation.
It is important to minimize exposure to sources of EMFs, such as cell phones, Wi-Fi routers, and other electronic devices, to reduce the potential risk of chronic pain and other health issues.
So, chronic pain syndrome is a complex condition that involves various factors, including changes in the nervous system, emotional factors, genetics, and lifestyle factors.
Integrative medicine to treat chronic pain
By understanding these factors, healthcare providers develop a multimodal approach called integrative medicine to the treatment of chronic pain. It includes allopathy and traditional medicines like yoga and ayurveda that addresses the underlying causes of the pain and promotes overall well-being.
How yoga and ayurveda can be effective for chronic pain?


Yoga and Ayurveda look for the root of the symptom. Even though the combination of allopathic and traditional medicine gives excellent results, the flaw of allopathic medicine is that it treats the symptom without seeking the cause. It is therefore necessary, in certain pathologies, to combine the two to obtain an effective treatment. Once the root of the problem is found, a protocol of mental, physical and spiritual practices is implemented with the patient.
It should be noted, however, that many disorders or diseases can be avoided through prevention, awareness, and intervention at the first stage of the disease, through yoga and ayurveda.
Symptoms of chronic pain syndrome
They can vary widely and may include persistent pain that can be dull, achy, sharp, shooting, or burning in nature. Other common symptoms can include fatigue, sleep disturbances, mood changes, and difficulty concentrating. Because chronic pain syndrome can be a complex condition with a wide range of symptoms, effective treatment often requires a multimodal approach that addresses both the physical and psychological factors contributing to the pain.
The effectiveness of yoga in the management of chronic pain
Yoga is a holistic practice that incorporates physical postures, breathing techniques, and mindfulness practices, all of which can help to reduce stress, promote relaxation, and improve physical function.
Several studies (see them in the references chapter below) have shown that yoga can be an effective therapy for the management of chronic pain by reducing it, improving neuromechanical and biochemical functions such:
- Lower back pain
- Neck pain
- Osteoarthritis
- Fibromyalgia
- Migraines
- Rheumatoid arthritis.
- Hormonal issues due to neurotransmitters imbalances
Yoga alleviate chronic pain by reducing inflammation in the body because chronic pain is often associated with inflammation And yoga practices reduce inflammation in the body.
Additionally, many types of chronic pain cited above, such as back pain, can be exacerbated by poor posture and reduced mobility. Yoga postures improve flexibility, strengthen the muscles that support the spine, promote better alignment either in the mind than physically, all of which can help to reduce pain and improve physical function.
How yoga reduce inflammation in the body
By reducing stress.
Stress triggers the release of cortisol and other stress hormones, which can cause inflammation in the body. By reducing stress, yoga is able to reduce inflammation as well.
Certain yoga poses like forward bends, twists, and inversions help to reduce inflammation in the body. These poses stimulate the parasympathetic nervous system, which can help to reduce stress and inflammation. Some examples include Child’s Pose (Balasana), Cobra Pose (Bhujangasana), and Legs Up the Wall Pose (Viparita Karani).
Also pranayama with deep breathing practices such as alternate nostril breathing (nadi shodhana) and bellows breath (bhastrika) have been shown to increase vagal tone and reduce inflammation in the body.


By increasing mindfulness.
Yoga practices such as meditation and deep breathing increase mindfulness and awareness of the present moment. This helps to reduce and master negative emotions such as anxiety and depression, which have been linked to increased inflammation.
Mindfulness meditation practices: scan meditation and loving-kindness meditation have been shown to reduce inflammation markers in the body.
By improving sleep.
Sleep is important for regulating the immune system and reducing inflammation. Yoga is helpful for improving sleep quality, which in turn can help to reduce inflammation.
Yoga nidra is a guided practice that involves a systematic relaxation of the body and mind. It has been shown to reduce inflammation markers in the body.
By stimulating the vagus nerve.
The vagus nerve is a key regulator of the immune system and inflammation. Some yoga practices, such as deep breathing and specific poses stimulate the vagus nerve which reduce inflammation.
By reducing weight:
Yoga help for reducing body weight and BMI, and balance hormonal disruptions which are associated with increased inflammation.
As I can see with my practicionner, Yoga and specific technics activate their relaxation response by activating the parasympathetic nervous system. It is responsible for the “relaxation response.” When the relaxation response is activated, their bodies switches from the “fight or flight” response to a state of deep relaxation. This shift helps to reduce their stress and inflammation.
Because Yoga reduce the levels of stress hormones in the body. It enhances sleep quality which is important for regulating the immune system and reducing inflammation. The immune system plays a key role in regulating inflammation.
Overall, Yoga have powerful effects on the nervous system and reduce inflammation in the body by promoting:
- relaxation,
- reducing stress,
- improving sleep quality,
- increasing mindfulness,
- and boosting immune function,
- and correcting the mind and physical postures.
Ayurveda: another golden key to fight chronic pain


If you read me, you know that I always link my articles’ topic with Yoga and Ayurveda. Those both sisters sciences lead to wonderful results and we really should apply their principles in our lives.
As a reminder Ayurveda is the Indian traditional system of medicine based on the concept of balance between mind, body, and spirit. Ayurvedic remedies for chronic pain are tailored to the individual’s specific needs. And specifically to it prakriti (personal ayurvedic constitution).
According to Ayurveda, chronic pain can be caused by an imbalance in any of the three doshas – Vata, Pitta, or Kapha. Each dosha is associated with specific qualities and functions in the body, and an imbalance in any of these can lead to chronic pain.
Role of doshas in chronic pain syndrom
Vata dosha is associated with movement and communication in the body, and an imbalance in Vata can cause dryness, coldness, and instability. Vata imbalances can lead to conditions such as arthritis, fibromyalgia, and nerve pain.
Pitta dosha is associated with metabolism and digestion, and an imbalance in Pitta can cause heat, inflammation, and acidity. Pitta imbalances can lead to conditions such as migraines, headaches, and inflammatory pain.
Kapha dosha is associated with structure and stability in the body, and an imbalance in Kapha can cause heaviness, congestion, and stagnation. Kapha imbalances can lead to conditions such as joint pain, osteoarthritis, and lymphatic congestion.
The approach that we use in Ayurveda to managing chronic pain syndrome involves identifying the doshic imbalances. That may be contributing to the pain and developing a personalized treatment plan that addresses these imbalances.
Our treatment plan may include dietary and lifestyle changes, herbal remedies, body therapies, yoga and meditation practices. All that are tailored to the patient’s unique constitution and imbalances.
Some ayurvedic remedies tips?
I give you some examples of Ayurvedic remedies for chronic pain that can include:
Turmeric: Turmeric is a spice that is commonly used in Ayurvedic medicine to reduce inflammation in the body. It contains a compound called curcumin, which has been shown to have anti-inflammatory properties.
Ginger: Ginger is another spice that is commonly used in Ayurvedic medicine to reduce pain and inflammation. It contains compounds called gingerols and shogaols, which have been shown to have anti-inflammatory and analgesic properties.


Massage: Ayurvedic massage, known as abhyanga, can help to reduce pain and promote relaxation. The massage is typically performed using warm herbal oils that are chosen based on the individual’s specific needs.
Yoga: As mentioned above, yoga can be an effective therapy for the management of chronic pain. Ayurvedic yoga, known as hatha, vinyasa yoga, is a type of yoga that is specifically tailored to the individual’s dosha, or body type.
In conclusion, chronic pain syndrome is a complex condition that can have a significant impact on an individual’s quality of life.
A multimodal approach that includes complementary therapies such as yoga and Ayurveda may help to alleviate pain, improve physical function, and promote overall well-being.
As always, anyone with chronic pain should consult with their healthcare provider before starting a new exercise program or complementary therapy.
References
Yoga as a treatment for chronic low back pain
Effectiveness of Yoga Intervention for Chronic Neck Pain
Efficacy of a biomechanically-based yoga exercise program in knee osteoarthritis
The Yoga of Awareness program in the management of fibromyalgia
Role of Yoga in Cancer Patients
Yoga for Treating Rheumatoid Arthritis
Occupational exposure to extremely low-frequency magnetic fields and the risk of ALS
…